After many years of ideation and dreaming of a better healthcare system, we've decided to take a leap of faith and dive head-first into solving the problems everyday Americans face by officially launching Winston Health!
Our mission is simple; help employers and employees work together to lower healthcare costs and improve health outcomes. To make progress toward our mission we need to build trust with our users so that they trust us to guide them along their health journey. As a first step in building that trust, we'll be writing a series of blog posts outlining how we got here and what motivates us to work hard to deliver a better healthcare system.
 Let's first start with our name, Winston Health. Our name comes from my pup, Winston. Winston is a 5-year-old "something-doodle", and in that time we've built an incredible bond and relationship. He is my shadow, my best friend, and my constant companion. When I go downstairs to watch TV, Winston follows. When I go into my office to work, he follows and keeps watch. Winston is more than a fearless and loyal companion though; he also helps motivate me to stay healthy with regular walks and runs around the neighborhood. Just as real-life Winston is for me, Winston Health strives to be that for our users, a loyal companion that you can rely on as you go through your health and healthcare journey. Naming our company and thinking of all of my great memories with Winston was fun, but the motivation for starting Winston Health goes deeper than that.
Let's first start with our name, Winston Health. Our name comes from my pup, Winston. Winston is a 5-year-old "something-doodle", and in that time we've built an incredible bond and relationship. He is my shadow, my best friend, and my constant companion. When I go downstairs to watch TV, Winston follows. When I go into my office to work, he follows and keeps watch. Winston is more than a fearless and loyal companion though; he also helps motivate me to stay healthy with regular walks and runs around the neighborhood. Just as real-life Winston is for me, Winston Health strives to be that for our users, a loyal companion that you can rely on as you go through your health and healthcare journey. Naming our company and thinking of all of my great memories with Winston was fun, but the motivation for starting Winston Health goes deeper than that.
In the fall of 2014, Drake and Post Malone were at the top of the Billboard charts and I was a freshman at Princeton University. The days were long and hot, my dorm didn't have AC (the not-so-glamorous part of attending a historic university they don't tell you about), and I was struggling to survive as a student-athlete.
A few weeks into the semester I began noticing non-trivial amounts of blood in my stool. At first, I thought it was a fluke and that it would go away, but as time passed, it didn't. One afternoon I went to McCosh Health Center, the university's student health services, to talk to a doctor about what was happening. After a brief examination, the doctor recommended I see a specialist. While not ideal, as I'd have to venture off campus, I agreed that it was probably best to get definite answers to my concerns.
Unfortunately, going to an off-campus doctor appointment was no easy task. At Princeton, students aren't allowed to have cars. I was also struggling to stay afloat in the intense, hyper-masculine environment of DI football. Between mandatory lifts, meetings, walk-throughs, practice, and film sessions, my schedule was monopolized by the football team. On top of this, I was getting playing time as a freshman and on the travel roster. This meant that Fridays and Saturdays were filled with travel and games. To cap it all off, my situation was no easy thing to talk about with my coaches, let alone commit heresy by asking to miss team time to go to a doctor's appointment.
Eventually, I mustered up the courage to share what was going on with my O-Line coach and I scheduled an appointment to see the specialist. When I arrived at the gastroenterologist's office I immediately knew that I was out of place. I can say, with 98% certainty, that I was the only person under 65 in the waiting room. Not ideal, but hey, the doctor is going to be great! Unfortunately, the doctor was a carbon copy of his patients: past retirement age, low energy, and unrelatable. When I left, I had a centerfold pamphlet, a script for something called a "suppository" (yikes!), and the knowledge that I had something called "Ulcerative Colitis" (UC).
At first, the suppositories worked and the blood in my stool went away, but fast forward a few months and I had fallen off a cliff, hard. My iron levels were in the tanks, I left toilet bowls looking like murder mystery props, and I was essentially incontinent. So, what turned a little blood in my stool into this?
I wasn't aware that Ulcerative Colitis is a chronic disease (you don't just "get better"), that I needed to take the medicine every day (forever), and the consequences of letting UC go untreated. On top of this, I was an immature 18-year-old with no money and parents who lived paycheck-to-paycheck, who as a child always thought "can we afford this" before asking to go to the doctor.
When I came home for winter break my sophomore year my Mom could tell something was wrong and she demanded to take me to get a second opinion. We went to Regional GI in Lancaster where I met Dr. John Betteridge. Dr. Betteridge was everything a doctor should be and gave me what I needed to get my disease under control. It has been nearly 10 years since I first saw Dr. Betteridge and I'm happy to say that I am in remission.
So, what's the point of me sharing this? Our current healthcare system failed me and my family. My life is forever changed, the quality of my life has been reduced, and the dreams I once had were taken from me because of it. In a better world, my disease would never have gotten worse, I would never have had to get a second opinion, I would never have felt too uncomfortable to talk to someone, and I would have never been afraid to seek care because of costs. But that's not how it happened because the system didn't and still doesn't work as it should. This is why we're starting Winston Health. This is what we're going to try, with all we have, to fix.
Now, I get it; my story is super unfortunate, but so are countless other personal stories. Why should anyone invest their time and attention in my story? What does it really matter? Simply put, my disease and current prognosis, the disease and prognosis that never had to happen, impacts all of us.
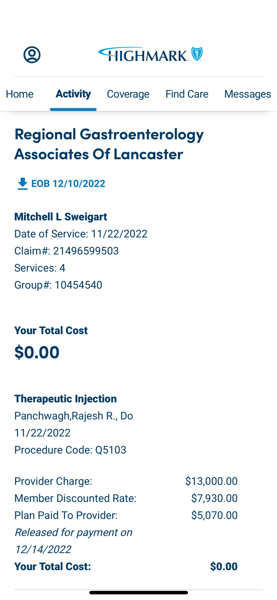
To get into and stay in remission I take REMICADE® (infliximab). Remicade isn't a "normal" medicine; it's administered to me intravenously (IV) over a 3 hour period every 8 weeks. It's also a maintenance drug, meaning that I'll be on this stuff for the rest of my life or until my body develops antibodies towards it and it becomes ineffective. The cherry on top is how STUPID expensive Remicade is, like $5,070 every eight weeks expensive (thank you Highmark app). When you consider my doctor visits, regular colonoscopies, quarterly full blood panels, and everything else, my disease costs my insurer north of $33,000 per year. Compared to a year's supply of Mesalamine suppositories, which I can get a 30-day supply for $80.81 at my local Walmart (thank you GoodRx <3), my disease costs $32,000 more per year than it should have.

And that isn't a cost that I or my insurer bear alone. It is a cost that we all bear. Really? Yeah, that's how insurance works; we all pay in premiums, the insurer pools our premiums together, and they pay our claims with the pool of money. If someone has high claims, the insurer raises everybody's premium to cover the bills. I'm 8 years into my disease and I've cost all of us $256,000 more than what I should have. It's unfortunate, but it's insurance 101.
Winston Health will always act in the best interest of people and their health, full stop. Fortunately, as my life demonstrates so perfectly, we don't need to rely on benevolence to convince people that encouraging health and prevention is a worthy pursuit. Said differently, if the average employer contributes 80/20 to their employee health insurance costs, they would have spent $204,800, which they didn't need to had I received the proper care, to cover me for the past 8 years.
Our journey is just beginning, but we couldn't be more excited. We've taken the first step in climbing Everest. A small milestone, but arguably one of the hardest parts. We hope that you join us in building a future we can all be proud of, where employees are their healthiest selves and employers enjoy the budgetary flexibility of health insurance that doesn't break the bank.
❤️🚀🐶